The gap between acquiring theoretical, classroom learning and translating that knowledge to care for patients has troubled medical education. Simulation allows learners at every level to develop and hone their physical, communication, and teamwork skills without putting a patient at risk. Standardized patients, who are actors, help learners practice communication and physical exam skills. Full-scale, standardized, electromechanical mannequins are programmed to mimic many different patient conditions and allow learners to practice diagnostic and treatments in a safe space. Various trainers are also used to teach procedural skills so learners have the opportunity to practice their skills before performing the procedure on a patient. Washington University School of Medicine employs simulation for all levels of learners in a variety of settings, optimizing the technology and the techniques for the task and the learners.


Medical student education is a primary focus of the simulation centers. In Phase 1, students spend time learning, practicing and being assessed in communication and physical assessment skills utilizing our Standardized Patients (SPs). In Phase 2’s clerkships, the students use both the SP’s and the simulation center to develop foundational skills before starting each clerkship. In Phase 3, we provide communication assessments as well as a Capstone course to assist the transition to residency.
Resident, fellow and inter-professional teams train in our simulation centers. We also provide educational programming for attending physicians and community physicians.
Surgical training is provided in the WISE Surgical Skills Lab which provides hands-on exercises that help teach a variety of surgical skills, including basic suturing, knot-tying, laparoscopic/endoscopic techniques and robotic surgery.
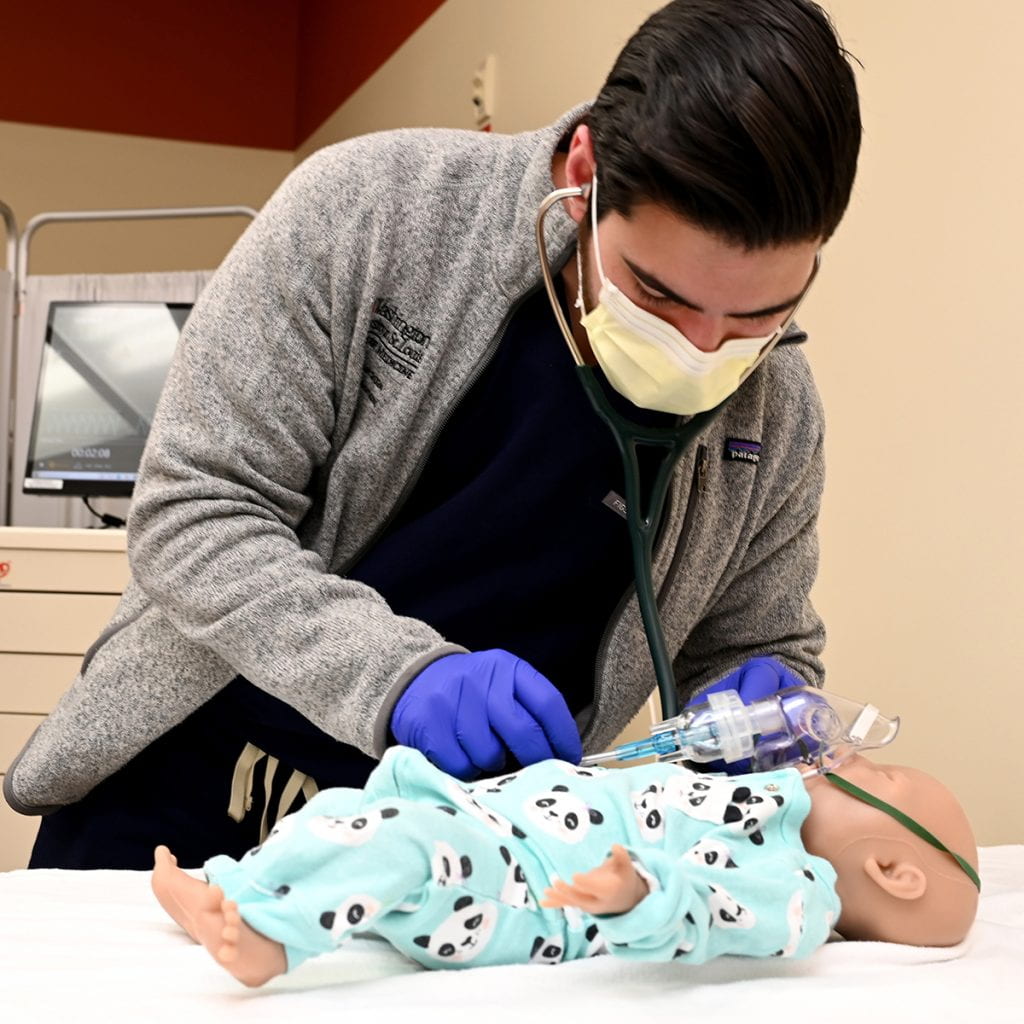
Pediatric training is provided in the Saigh Pediatric Simulation Center at St. Louis Children’s Hospital. The center provides training for nursing, fellows, residents, and medical students to improve skills in managing pediatric patients.